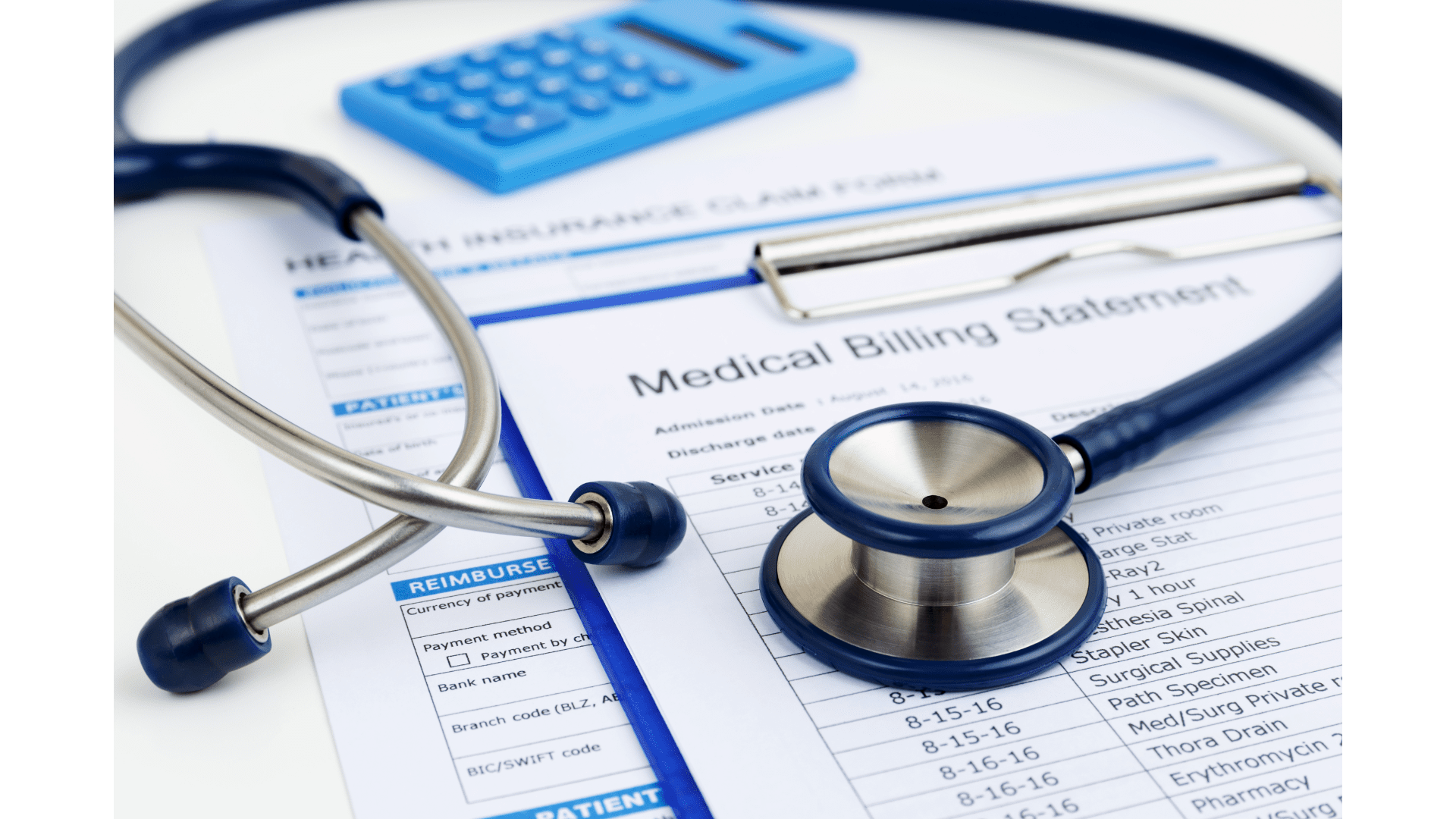
Outsourced Medical Billing Solutions For Secure & Faster Reimbursement
In today’s constantly evolving healthcare industry, running a medical practice can be a complex and demanding job. Between seeing patients, managing staff, and keeping up with administrative tasks, it can be difficult for healthcare providers to focus on financial aspects of their practice. While, the financial stability of the practice is very important and can only be acheived by a professional medical billing service to ensure accurate and timely reimbursement from the Insurances. Therefore, a professional medical billing service is a critical component of financial success for your healthcare practice.
Here are some of the key benefits of outsourced medical billing services:
Cost Effective
Outsourcing medical billing services can be more cost-effective than hiring and training in-house staff, purchasing billing software, and maintaining expensive equipment.
Time Savings
You can free up your in-house staff from the time-consuming task of handling billing and allow them to focus on more important tasks, such as caring for patients.
Compliance
Medical billing can be complex, and it’s essential to stay up-to-date with changes in regulations and payer requirements. Outsourced medical billing service can help ensure that your billing is in compliance with healthcare industry regulations and avoid costly errors that can result in denied claims.
Improved Cash Flow
An outsourced medical billing service can help you receive payments more quickly, improving your cash flow and reducing the financial strain on your practice.

Conclusion
The only way to ensure the financial stability of your practice and provide the highest level of care to your patients, is by maximizing your revenue, improving compliance, reducing administrative burden, and improving your cash flow. In recent years, due to constantly changing healthcare Industry and a dramatic increase in In-house staffing costs, outsourced medical billing services have become critical component of financial success for any healthcare practice. If you are looking for an outsourced medical billing company to help take your practice to the next level, please do not hesitate to contact us. At Advanced RCMS, our medical billing specialists will help you enhance your overall revenue cycle health while working constantly and effectively on any denied claims to avoid revenue loss. You can contact our sales department at [email protected] or visit our website www.advancedrcms.com. Also, you can call us at 786.406.9218. Our team of experts has the experience and expertise to help you maximize your revenue and achieve your financial goals.
Get in Touch
Please Fill out your details below with the service that you need, And We’ll get back to you As Soon As Possible.
The Importance of a Professional Website for Your Business: A Guide for Healthcare Providers
I
n today’s digital age, having a strong online presence is essential for any business. Your website is often the first point of contact between your business and potential clients, and it can play a significant role in the success of your business. A well-designed website can help establish credibility, increase visibility, provide a better user experience, and give you a competitive advantage over your competitors.
However, not all website designs are created equal. A poorly designed website can have the opposite effect and harm your business by creating a negative impression, decreasing visibility, and providing a poor user experience. That’s why it’s essential to invest in a good website design that meets the needs of your business and your clients.


Here are some of the key benefits of an attractive website design:
Increased Credibility
A well-designed website gives your business a professional image and helps establish credibility with your customers. It shows that you take your business seriously and that you are committed to providing a high-quality experience for your clients.
Improved User Experience
A good website design should be user-friendly and easy to navigate. It should provide your clients with the information they need quickly and efficiently, and it should be optimized for different devices, including desktop computers, laptops, and mobile devices.
Enhanced Visibility
A well-designed website should be optimized for search engines, making it easier for potential clients to find your services online. This can help increase visibility and drive more traffic to your website.
A Better Conversion Rate
A good website design can also help improve conversion rates by providing a clear call-to-action and making it easy for clients to take the desired action, such as making an appointment or contacting you for more information.

In short, a good website design is essential for any business that wants to establish credibility, increase visibility, and provide a better user experience for its customers. By investing in a well-designed website, you can give your business a competitive edge and help drive more success for your business. If you are looking for a WordPress web design and development company to help bring your vision to life, look no further than Advanced RCMS. Our team of experts can help you create a professional website that meets the needs of your business and your clients, and that helps you achieve your goals. Please feel free to contact us at [email protected], or visit our website www.advancedrcms.com. Also, you can call us at 786.406.9218 for further details.
Schedule An Appointment
Please Fill out your details below with the service that you need, And We’ll get back to you As Soon As Possible.
Medical Coding: An Overview
Medical coding is the process of converting diagnostic statements and procedures into standardized codes that are used for reimbursement and data analysis purposes. This process plays a crucial role in the healthcare industry as it helps to ensure that the appropriate amount is paid for the services provided and helps to keep medical records organized and up-to-date.
The Importance of Accurate Medical Coding
Accurate medical coding is essential in ensuring that healthcare providers receive the correct reimbursement for the services they have provided. Inaccurate coding can result in incorrect payment, denial of claims, and even legal consequences. This is why it is imperative that medical coding specialists are highly trained and up-to-date on the latest coding guidelines and regulations.
Types of Medical Codes
There are several types of medical codes that are used in the healthcare industry, including:
Current Procedural Terminology (CPT) codes:
CPT (Current Procedural Terminology) codes are standardized codes used to describe medical procedures and services performed by healthcare providers.
ICD (International Classification of Diseases) codes:
ICD (International Classification of Diseases) codes are used to describe diagnoses and medical conditions. These codes are used by medical billers and coders to accurately communicate information about medical procedures and conditions to insurance companies and government healthcare programs, and play a crucial role in determining payment for medical services.
Healthcare Common Procedure Coding System (HCPCS) codes:
HCPCS (Healthcare Common Procedure Coding System) codes are used to describe supplies and equipment used in patient care.
The Importance of Keeping Up-to-Date with Coding Changes
With constantly evolving healthcare industry, coding guidelines and regulations are also changing. It is important for medical coders to stay informed and up-to-date on the latest coding changes, as this can significantly impact the accuracy and success of their coding efforts.
The Benefits of a Professional Coder For Your Practice
Professional medical coders play a crucial role in the healthcare industry by accurately coding medical diagnoses and procedures for insurance billing purposes. The benefits of having a professional medical coder on your healthcare team include increased efficiency in the billing process, improved accuracy in coding, and increased reimbursement for the healthcare providers. By accurately coding medical diagnoses and procedures, professional medical coders can help reduce the risk of denied claims and improve the financial stability of the healthcare organization. Additionally, professional medical coders keep up to date with the latest coding guidelines and regulations, ensuring that the healthcare organization is in compliance with industry standards. The expertise of a professional medical coder can also help to identify areas for improvement in the healthcare organization’s coding and billing processes, leading to increased overall efficiency and profitability.
Continuing Education and Professional Development
To maintain coding skills and knowledge, medical coders must continuously educate themselves through continuing education and professional development opportunities. This can include attending coding conferences and participating in coding workshops, and earning certifications
Conclusion
Medical coding is a critical component of the healthcare industry that helps to ensure that medical providers receive the accurate and timely reimbursement for the services they have provided. Accurate coding is essential, and medical coders must stay informed and up-to-date on the latest coding changes and regulations. Through continuing education and professional development, medical coders can maintain their coding skills and knowledge and ensure the success of their coding efforts.
Schedule An Appointment
Please Fill out your details below with the service that you need, And We’ll get back to you As Soon As Possible.
Getting Timely and Accurate Reimbursements for out-of-network Bills

Getting reimbursed for out-of-network bills can be a challenge for healthcare providers, but there are steps they can take to increase their chances of receiving payment. Providers should verify insurance coverage, inform patients in advance of out-of-network costs, use accurate billing information and appropriate coding, file an appeal if necessary, negotiate with insurance companies, and consider utilizing a medical billing service. By following these steps, healthcare providers can navigate the complex reimbursement process and improve their chances of getting paid for the services they provide.
What are out-of-network medical bills?
Out-of-network medical bills occur when a patient receives medical care from a provider who is not part of his/her insurance plan. In this case, patient’s insurance company may only pay a portion of the bill, and the patient may be responsible for paying the rest.
Why do out-of-network medical bills happen?
Out-of-network medical bills can happen for several reasons. For example, a patient goes to an emergency room that is out-of-network or receives care from a specialist who is out-of-network provider. Additionally, the patient may see a doctor who is in-network, but receives services from a lab or facility that is out-of-network. In some cases, patients may choose to receive care from out-of-network providers because they are closer to them or because they offer specialized services that are not available from in-network providers.
How to maximize reimbursements for out-of-network medical billing claims?
Medical providers can receive maximum reimbursement for out-of-network medical billing claims by following certain best practices and taking proactive steps to manage the billing process. Here are some tips for healthcare providers to maximize reimbursements for out-of-network claims:
Verifying insurance coverage
Verify the patient’s insurance coverage before providing services. This can help you understand what the patient’s insurance policy covers and what the patient is responsible for paying.
Billing accurately
Bill accurately for all services provided, using the correct codes and descriptions. This can help ensure that you receive full reimbursement for your services and can also reduce the risk of denied claims.
Following up on denied claims
Follow up on denied claims promptly and appeal if necessary. This can help ensure that you receive the full reimbursement you are entitled to and can also reduce the risk of delayed payments.
Negotiating with insurance companies
Consider negotiating with insurance companies for faster reimbursements. This can help you receive fair compensation for your services and can also help you build a strong working relationship with insurance companies.
Keeping up to date with insurance policies
Stay up to date with insurance policies and regulations. This can help you understand the reimbursement process and ensure that you are following all relevant regulations.
Hiring a medical billing specialist
Consider hiring a medical billing specialist who can manage the billing process on your behalf. This can help ensure that claims are submitted accurately and promptly, and that you receive maximum reimbursement for your services.
Medical providers can receive maximum reimbursement for out-of-network medical billing claims by verifying insurance coverage, billing accurately, following up on denied claims, negotiating with insurance companies, keeping up to date with insurance policies, and hiring a medical billing specialist. By taking these proactive steps, medical providers can help ensure that they receive the compensation they deserve for their services. If you are an out-of-network provider looking for outsourced medical billing services to improve the financial performance of your practice while reducing administrative costs, you are at the right place! At Advanced RCMS, our medical billing specialists can help you to receive maximum reimbursement for out-of-network medical bills by utilizing their knowledge of insurance policies and regulations, submitting accurate and timely claims, negotiating with insurance companies, and appealing denied claims to ensure that the providers receive the full compensation they are entitled to. Please contact us today at [email protected], or visit our website, www.advancedrcms.com. Also, you can call us at 786.406.9218 for further details regarding our services.
Schedule An Appointment
Please Fill out your details below with the service that you need, And We’ll get back to you As Soon As Possible.
Introduction to Provider Credentialing and Contracting
In the healthcare industry, provider credentialing and contracting are two crucial processes that ensure that healthcare providers are qualified, competent, and meet certain standards. These processes are vital in safeguarding the quality of care delivered to patients and ensuring that providers are reimbursed appropriately for their services. In this blog, we will discuss provider credentialing and contracting in detail, their importance, and the key factors to consider when choosing a provider credentialing and contracting company.
What is Provider Credentialing?
Provider credentialing is the process of verifying and documenting the education, training, licensure, and work history of a healthcare provider. It involves checking the provider’s background, malpractice history, and professional references. The goal of provider credentialing is to ensure that healthcare providers meet the minimum qualifications and standards set by healthcare organizations, insurance companies, and government agencies.

The provider credentialing process typically includes the following steps:
Provider application:
Providers fill out an application that includes information about their education, training, licensure, work history, and other relevant information and submit it to the Insurance company.
Verification of credentials:
The Insurance company verifies the information provided by the providers, including education, training, licensure, work history, and any malpractice history.
Background check:
Then the Insurance company conducts a background check to ensure that the providers have not been convicted of any crimes that could affect their ability to provide safe and effective healthcare.
Professional references:
In the next step, the professional references are verified to check the provider’s work history and reputation.
Review of the provider’s file:
The Insurance company reviews the provider’s file to ensure that all required documentation is present and accurate.
Approval or denial:
In the last phase of credentialing process, Insurance company either approves or denies the provider’s credentialing application based on the information gathered during the verification process.
What is Provider Contracting?
Provider contracting is the process of negotiating and executing contracts between healthcare providers and insurance companies, government agencies, or other healthcare organizations. The goal of provider contracting is to establish the terms and conditions under which a healthcare provider will be reimbursed for their services.
The provider contracting process typically includes the following steps:
Negotiations: The provider and the healthcare organization negotiate the terms and conditions of the contract, including reimbursement rates, covered services, and any other relevant terms.
Contract execution: Once the terms and conditions have been agreed upon, the contract is executed, and both parties sign the document.
Contract management: The Insurance company manages the contract, ensuring that the terms and conditions are met, and that the provider is reimbursed appropriately for their services.
Why is Provider Credentialing and Contracting Important?
Provider credentialing/contracting is important for several reasons, including:
Quality of care: Provider credentialing ensures that healthcare providers meet certain minimum qualifications and standards, which helps to ensure that patients receive safe and effective care.
Reimbursement: Provider contracting establishes the terms and conditions under which a healthcare provider will be reimbursed for their services, ensuring that providers are reimbursed appropriately for the care they deliver.
Compliance with regulations: Provider credentialing and contracting help healthcare organizations comply with regulations set by insurance companies, government agencies, and other organizations.
Patient safety: Provider credentialing and contracting help to ensure that healthcare providers have no history of malpractice or criminal activity, which helps to protect patients from potential harm.
Key Factors to Consider When Choosing a Provider Credentialing and Contracting Company
When choosing a provider credentialing and contracting company, it is important to consider the following factors:
Experience: Look for a company that has a proven track record of success in provider credentialing and contracting. Make sure they have experience working with healthcare providers and organizations in your specialty and geographic area.
Quality of services: Choose a company that offers comprehensive and thorough provider credentialing and contracting services. The company should be able to handle all aspects of the process, from verification of credentials to contract management.
Turnaround time: Consider a company that has a fast and efficient turnaround time for provider credentialing and contracting. This will ensure that healthcare providers are able to start seeing patients and receiving reimbursement for their services as soon as possible.
Customer service: Choose a company that has a strong reputation for excellent customer service. They should be responsive and accessible, and able to answer any questions or concerns you may have throughout the process.
Technology and automation: Consider a company that uses technology and automation to streamline the provider credentialing and contracting process. This will help to minimize errors and reduce turnaround time.
Cost: Look for a company that offers competitive pricing for their services. Make sure to compare prices and services offered by multiple companies to find the one that best fits your needs and budget.
Provider credentialing and contracting are crucial processes in the healthcare industry that help to ensure the quality of care delivered to patients and ensure that healthcare providers are reimbursed appropriately for their services. When choosing a provider credentialing and contracting company, it is important to consider their experience, quality of services, turnaround time, customer service, technology and automation, and cost. By choosing a company that meets these criteria, healthcare organizations and providers can have peace of mind knowing that their credentialing/contracting is in good hands.
At Advanced RCMS, we are dedicated to providing comprehensive and efficient provider credentialing and contracting services to help healthcare providers get Credentialed/Contracted with their most desired healthcare Insurances to be able to deliver quality care to their patients while receiving fair and timely reimbursement from healthcare Insurances for their services. For further details regarding our services, please contact us today at [email protected], or visit our website www.advancedrcms.com. You can also call our sales department at 786.406.9218.
Schedule An Appointment
Please Fill out your details below with the service that you need, And We’ll get back to you As Soon As Possible.
Hiring a Medical Virtual Assistant: An In-Depth Guide
In today’s fast-paced world, medical professionals are finding it increasingly difficult to manage their workload and keep up with their patients’ demands. This is where medical virtual assistants come in – they can help with administrative tasks, freeing up time for medical professionals to focus on providing care to their patients. In this blog, we will take a detailed look at what a medical virtual assistant is, what skills they need to have, and the benefits of hiring one.
What is a Medical Virtual Assistant?
A medical virtual assistant is a professional who works remotely to provide administrative support to medical professionals. They handle tasks such as scheduling appointments, managing patient records, responding to emails, etc,. Medical virtual assistants can work for a single medical professional or for a larger healthcare organization.

What Skills Should a Medical Virtual Assistant Have?
Medical Terminology:
Medical virtual assistants need to have a good understanding of medical terminology and be able to use it accurately. This is crucial in ensuring that patient records and other medical documents are properly maintained and updated.
Attention to Detail:
Medical virtual assistants need to be detail-oriented and meticulous in their work. They need to be able to catch any errors and ensure that patient information is accurate and up-to-date.
Communication Skills:
Medical virtual assistants need to have excellent written and verbal communication skills. They need to be able to communicate effectively with patients, healthcare professionals, and other members of the healthcare team.
Technical Skills:
Medical virtual assistants need to be proficient in using various software and tools, such as electronic health record (EHR) systems and appointment scheduling software.
Organization and Time Management:
Medical virtual assistants need to be highly organized and able to manage their time effectively. They need to be able to prioritize tasks and meet deadlines.

Benefits of hiring a Medical Virtual Assistant
Hiring a medical virtual assistant can bring numerous benefits to healthcare providers and their patients. In today’s fast-paced healthcare industry, virtual medical assistants can offer a cost-effective and efficient solution to many of the administrative and clinical challenges faced by healthcare providers. In this blog, we will explore the benefits of hiring a medical virtual assistant.
Increased Efficiency:
One of the most significant benefits of hiring a medical virtual assistant is increased efficiency. Virtual medical assistants can handle routine administrative tasks such as appointment scheduling, record keeping, and patient communication, freeing up time for healthcare providers to focus on patient care. This can lead to a more streamlined workflow, reduced wait times for patients, and an overall improvement in the quality of care provided.
Cost-effective Solutions:
Hiring a virtual medical assistant can also result in significant cost savings for healthcare providers. Unlike traditional in-house medical assistants, virtual medical assistants do not require benefits, office space, or training. This can help healthcare providers to reduce costs and improve their bottom line.
Improved Patient Care:
Medical virtual assistants can also play a very important role in improving patient care. They can provide patients with quick access to information and support, answer questions, and assist with telemedicine consultations. This can lead to improved patient satisfaction and a better overall healthcare experience.
Flexibility:
Another benefit of hiring a medical virtual assistant is the flexibility. Virtual medical assistants can work from anywhere and at any time, making them a cost-effective solution for healthcare providers who need support during peak periods. This can help to reduce the workload of in-house staff and ensure that patients receive the care they need, when they need it.
Expertise:
Medical virtual assistants can also bring a high level of expertise to healthcare providers. They are trained and qualified to handle a wide range of administrative and clinical tasks, and can provide valuable support to healthcare providers. This can help to improve patient care and ensure that healthcare providers have access to the resources they need to provide the best possible care.
In conclusion, hiring a medical virtual assistant can bring numerous benefits to healthcare providers and patients. From increased efficiency and cost savings, to improved patient care and access to expertise, virtual medical assistants can offer a cost-effective and efficient solution to many of the challenges faced by healthcare providers. If you are looking for a way to improve the quality of care you provide and reduce costs, a medical virtual assistant may be the solution you need.
At Advanced RCMS, we are dedicated to providing highly qualified virtual medical assistance services to healthcare providers and their patients. With a team of highly trained and qualified virtual medical assistants, we help providers to improve overall efficiency, reduce costs, and enhance the quality of care provided. Please do not hesitate to contact us for further details regarding our services at [email protected], or visit our website www.advancedrcms.com. Also, you can call us at 786.406.9218 and our dedicated staff will be more than happy to assist you.
Schedule An Appointment
Please Fill out your details below with the service that you need, And We’ll get back to you As Soon As Possible.






